Sudden infant death syndrome or SIDS is the most common form of death for post neonatal infants in the developed world, with thousands of SIDS deaths every year worldwide. SIDS remains a non-definable diagnosis. Despite a thorough investigation by police and the coroner, there are no clear answers for parents who have lost a child. Why do seemingly healthy infants stop breathing during sleep and fail to wake up? Failure of arousal and cessation of breathing are also common symptoms of other sleep-related disorders such as obstructive sleep apnoea, which affects 1 in 80 children and over a million adults in Australia.
Mr Nicholas Hunt, Dr Rita Machaalani and Prof. Karen Waters at the University of Sydney (USyd) are examining the neurological connections that induce arousal. These are complex with several neuropeptides critical to the arousal function. Using the AMMRF (now Microscopy Australia) at the USyd this group has shown that one of these neuropeptides, orexin, is reduced by 20% in SIDS babies. This loss of orexin also occurs in infant animal models of SIDS. These animals also demonstrated impaired arousal following cessation of breathing or exposure to elevated carbon dioxide and reduced oxygen (hypercapnic hypoxia), a prominent risk factor for SIDS generated by prone sleeping. In a previous study they also showed that exposure to hypoxia reduced the production of orexin in baby animals. The team’s current studies are examining the mechanism by which this occurs. Initial data suggests it is mediated by the modification of a protein called PERK, which reduces the production of a whole suite of proteins.
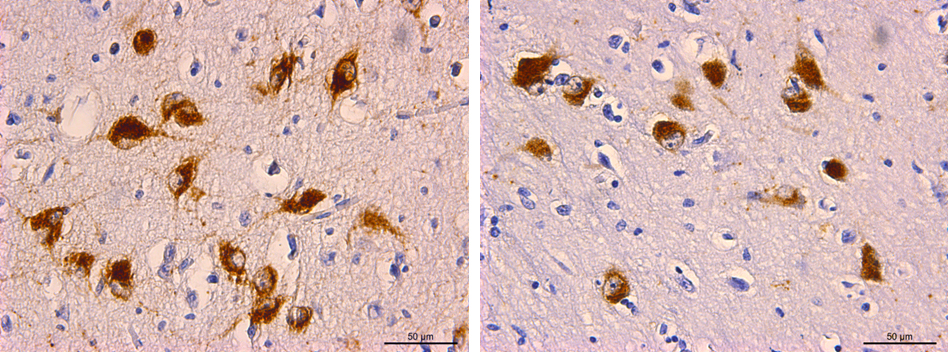
Light micrograph showing orexin-stained neurons in brown. Normal infant brain, left, and a SIDS infant brain, right.
These studies establish a direct pathway between risk factors for SIDS and the regulation of sleep and arousal so vital to an infant’s survival. The pathway for reduced production of orexin in SIDS has broader implications for childhood and adult sleep-related disorders such as obstructive sleep apnoea, where reduced orexin levels have also been seen, and where hypercapnic hypoxia is also an issue. Orexin may also play a role in neurological disorders like Alzheimer’s and Parkinson’s that have secondary sleep dysfunction as the diseases progress.
Having identified the pathway connecting hypercapnic hypoxia to reduced numbers of orexin neurons and reduced arousal, it may soon be possible to save lives and improve the quality of sleep for millions of people by:
Ref. N. Hunt et al., Acta Neuropathol., 130(2), 185, 2015
Ref. N. Hunt et al., Neuropathology of Aging, 36(2), 292, 2015
September 21, 2015